Assessment and Management of Bruxism by certificated CRAFTA® Physical Therapists
Introduction
Over the last two decades the classification and definition of bruxism has been adapted and changed because of the complexity and the minor evidence of the mechanism behind bruxism. In 2013 an international consensus of dentistry experts (International Network for Orofacial Pain and Related Disorders Methodology (INfORM) of the International Association Dental Research (IADR)) met and a grading system was proposed.
It was refined in 2018 together with an assessment proposal (Lobbezoo et al 2018). In 2019 The German associations Deutsche Gesellschaft für Funktionsdiagnostik und -Therapie in der Zahn-, Mund- und Kieferheilkunde (DGFDT) and Deutsche Gesellschaft für Zahn-, Mund- und Kieferheilkunde (DGZMK), performed a literature review and published a guideline about the management of bruxism which is a deepening of the review of Lobezoo et al 2008. The actual definitions from the INfORM are:
Bruxism is repetitive masticatory muscle activity characterized by clenching or grinding of the teeth and/or by bracing or thrusting of the mandible and specified as either sleep bruxism or awake bruxism. (Lobbezoo et al 2013)
- Sleep bruxism (SB) is a masticatory muscle activity during sleep that is characterized as rhythmic(phasic) or non-rhytmic (tonic) and is NOT a movement or sleep disorder in otherwise healthy individuals.
- Awake bruxism (AB) is a masticatory muscle activity during wakefulness that is characterized by repetitive or sustained tooth contact and/or by bracing or thrusting of the mandible and is NOT a movement disorder in otherwise healthy individuals.
(Lobbezoo et al International Consensusgroup 2018)
The consensus group concluded that bruxism is a disorder and not a disease with a high level of masticatory muscle activity which may increase the risk of negative oral health consequences, severe masticatory muscle and or temporomandibular joint pain, extreme mechanical tooth wear and prosthodontic complications (Abe et al 2009, Manfredini et al. 2008, 2014). Risk factors for bruxism may be classified in occlusion factors or clinical factors e.g Temporal Mandibular Disorder (TMD) and psychological factors (Lobbezoo et al 2018)
Assessment of Bruxism of a specialized physical therapist (CRAFTA certificated)
A CRAFTA therapist assessment will conform as much as possible to the consensus group, INfORM, which suggests that there will be a large overlap with assessment of the dentist. The domain will always be the (neuro)musculoskeletal system, analyzing the individual risk factors which may be useful in understanding the clinical pattern of bruxism and for possible management strategies. A short overview is discussed below.
(a)Non-Instrumental Approach
- Self-reported assessment of sleep or awake bruxism continues to be the primary tool in bruxism research and clinical practice more than a instrumental approaches (Lobbezoo et al 2018). Appropriate screening protocols like Neck Disability Index (NDI), Jaw Disability Index(JDI) and Conti Questionnaire (AQ) may support neck-jaw function and presence of TMD. A specials questionnaire has been developed for research and clinic to give an idea if AB and/or SB is present called the Bruxism Status questionnaire(BSQ) (von Piekartz et al. 2019). For a copy of the BSQ see (Link).
- Inspection of the extra-oral (face) and intra-oral. The tooth wear evaluation system (TWES) )(Wetselaar & Lobbezoo 2016) can be concocted in consensus with the dentist.
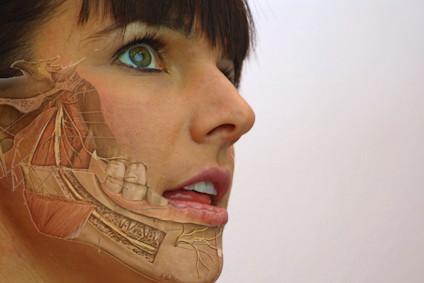
- Physical screening of the orofacial-cervical region. Assessment of active and passive movements of the temporal mandibular joint (TMJ) and the cervical spine to analyze TMJ and cervical impairments (especially the upper cervical region) and pain experience.
- Orofacial motor control Assessment. The purpose is to investigate and analyze the subtitle motor function related with(out) pain experience during performance of the movement (contributing factor ?). The assessments are divided in two categories:
a.Specific Functional Assessments: - Systematic tongue and lip movements
- Swallowing and breathing function like the Tongue Teeth Breathing Swallowing (TTBS) assessment
- Habitual Reversal (HR): relaxation of the orofacial muscles on command with or without reciprocal stimuli
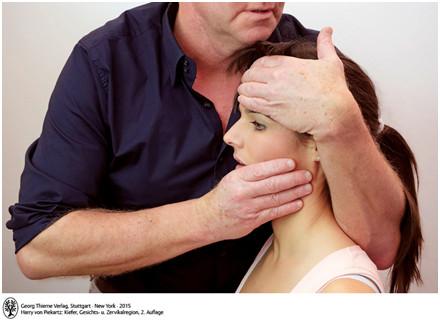
- Brace Relax Technique (BRT): Passive oscillatory movement by the clinician while assessing the motor response of the masticatory muscles.
- b. Orofacial-cervical motor control tests
- A battery of 8 tests used as a clinical tool to identify patients with reduced motor control in the craniofacial region (von Piekartz et al. 2017).
Most assessments may be directly imbedded in musculoskeletal management of (awake) Bruxism (see below)
(b)Instrumental Approach
- Electromyographic (EMG) recordings, somnography or polysomnography (Audio and/or video recordings (in combination with EMG) is in not commonly executed by a physical therapist unless she/he is working as part of a special team.
Reflection after the Non-Instrumental Assessment
- • Is there clear Bruxism (awake vs sleep)?
- • Is there a clear TMD comorbid with bruxism?
- • Are there clear cervical impairment associated with the main symptoms?
- • Is there a clear trigeminal sensitivity?
- unilateral vs bilateral
- Face vs cervical
- What are the individuals risk factors – contributing factors?
- Are there actual red flags requiring a referral to medical doctor?
- Is a positive outcome in management of bruxism with physical therapy expected?
- Is a referral or cooperation to/with a dentist or other healthcare providers needed?
Management
The German associations DGFDT and DGZMK divided their Management of Bruxism guidelines into four approaches; a)Occlusal/dentistry, b)Pharmacological, c)Psychological/behavioral and d)Musculoskeletal/physical therapy.
The outcomes with Musculoskeletal/physical therapy are satisfying to good when a combination of manual therapy and complementary remedies such as cold or heat treatments are considered for the treatment of TMD symptoms that may be triggered by bruxism. AB patients should be instructed on how to perform awareness and/or mindfulness exercises and/or relaxation techniques for self-management (E 3 Guideline 2019) Reflecting on this knowledge a specialized CRAFTA physical therapist will follow the next management guidelines.
- Reducing ongoing nociception in the oro-facial-cervical region by manual therapy, exercises to reduce trigeminal sensitivity which may have influence TMD and motor control during AB.
Note that bruxism and severity of TMD are independent predictors for pain and neck pain during movements and in most cases not are related with cervical impairments (von Piekartz et al 2019) - Motor-control exercises with a cognitive-behavior context such as the TTBS,HRT and BRT exercises.
- Individual life style changes by being aware during pain related activities with AB symptoms.
- Bruxism/Pain education (see also statement Pain education)
- Ecological momentary assessment /management of AB; Brux app ( Android and IOS) (Bracci et al 2018).
- Pain management strategies graded activity and/or graded exposure may be integrated .
- Cooperation /consensus with dentist, psychologist of help providers when necessary
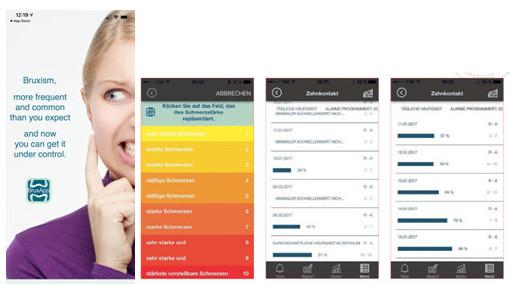
Brux App may support behavior changes in awake Bruxism and may be a part of Bruxism education (Bracci et al 2018)
Summary
- Sleep and Awake Bruxism is a disorder with several risk factors like increased muscle activity , mental stress , TMD and pain which may be positively influenced a CRAFTA physical therapy.
- A CRAFTA specialized physical therapy will be driven by the Bruxism’s consensus group INfORM as described above.
Literature
- Abe S, Yamaguchi T, Rompré PH, De Grandmont P, Chen YJ, Lavigne GJ. Tooth wear in young subjects: a discriminator between sleep bruxers and controls? Int J Prosthodont. 2009;22:342-350
- Bracci, A., Lange, M., Djukic, G., Guarda-Nardini, L., & Manfredini, D. Ecological momentary assessment of awake bruxism behaviors. Zeitschrift für Kraniomandibuläre Funktion, 2018 10(3), 217-228.
- German Society of Craniomandibular Function and Disorders (DGFDT),German Society of Dental, Oral and Craniomandibular Sciences (DGZMK) S3 Guideline (ect version) Bruxismus Diagnosis and Treatment, J. of Craniomand. Function 2019;11(3):225–i385
- Lobbezoo, F., Van Der Zaag, J., Van Selms, M. K. A., Hamburger, H. L., & Naeije, M. Principles for the management of bruxism. Journal of oral rehabilitation, 35(7),2008, 509-523.
- Lobbezoo F, Ahlberg J, Glaros AG, et al. Bruxism defined and graded: an international consensus. J Oral Rehabil. 2013;40:2-4
- Lobbezoo, F., Ahlberg, J., Raphael, K. G., Wetselaar, P., Glaros, A. G., Kato, T., ... & Koyano, K. International consensus on the assessment of bruxism: Report of a work in progress. Journal of oral rehabilitation, 45(11), 2018,837-844.
- Manfredini D, Lobbezoo F. Relationship between bruxism and temporomandibular disorders: a systematic review of literature from 1998 to 2008. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109:e26-e50.
- Manfredini D, Poggio CE, Lobbezoo F. Is bruxism a risk factor for dental implants? A systematic review of the literature. Clin Implant Dent Relat Res. 2014;16:460-469.
- Manfredini D, Guarda-Nardini L, Marchese-Ragona R, Lobbezoo F. Theories on possible temporal relationships between sleep bruxism and obstructive sleep apnea events. An expert opinion. Sleep Breath. 2015;19:1459-1465.
- Raphael KG, Janal MN, Sirois DA, et al. Validity of self-reported sleep bruxism among myofascial temporomandibular disorder pa- tients and controls. J Oral Rehabil. 2015;42:751-758
- Von Piekartz H, Physikalische Untersuchung von Dysfunktionen der kraniomandibuläre Region Kiefer ,Gesichts-und Zervikal Region , Thieme Stuttgart, 2017,150-164
- Von Piekartz, H., Stotz, E., Both, A., Bahn, G., Armijo‐Olivo, S., & Ballenberger, N. (2017). Psychometric evaluation of a motor control test battery of the craniofacial region. Journal of oral rehabilitation,2017 44(12), 964-973.
- Von Piekartz, H., Rösner, C., Batz, A., Hall, T., & Ballenberger.Bruxism, temporomandibular dysfunction and cervical impairments in females–Results from an observational study. Musculoskeletal Science and Practice, 2019, 45, 102073.
- Wetselaar P, Lobbezoo F. The tooth wear evaluation system (TWES): a modular clinical guideline for the diagnosis and management planning of worn dentitions. J Oral Rehabil. 2016;43:69-80

Manual Cranial Therapy
Cranial manual therapy means: assessment and treatment of the cranium..
Read more..

Pain Education
“pain neuroscience education (PNE)” or “Explain Pain” is a therapeutic tool...
Read more..

Headache (HA) in children
What can the (specialized) physical therapist mean for this pain suffering group..
Read more..

Assessment Bruxism
Assessment and Management of Bruxism by certificated CRAFTA® Physical Therapists
Read more..
Clinical classification of cranial neuropathies
Assessment and Treatment of cranial neuropathies driven by clinical classification..
Read more..

Functional Dysphonia
Functional Dysphonia (FD) is a condition characterized by voice problems in the absence of a physical laryngeal pathology.
Read more..

Body Image and Distorted Perception
Body Image and Distorted Perception of One's Own Body – What Does This Mean?
Read more..

TMD in Children
TMD affects not only adults, but it also occurs frequently in children and adolescents..
Read more..


